World’s first “electric band-aid” for non-healing wounds
Ph.D. Candidate in Biomedical Engineering of Northwestern University, Joseph W. Song, is introducing the world’s first “electric band-aid.”
This is an electrotherapy device that will accelerate the healing process of non-healing wounds. Wounds such as diabetic ulcers and pressure ulcers are categorized as non-healing. These wounds need to be healed as fast as possible, as infection is likely and dangerous.
“Because they have irregular homeostasis, their wounds just don’t heal. It’s because of bacterial infection and also the pressure applied to the foot ulcers,” Song said. “So, using this device we can encapsulate the healing process by accelerating the migration of epithelial cells from the healthy site to the injured site.”
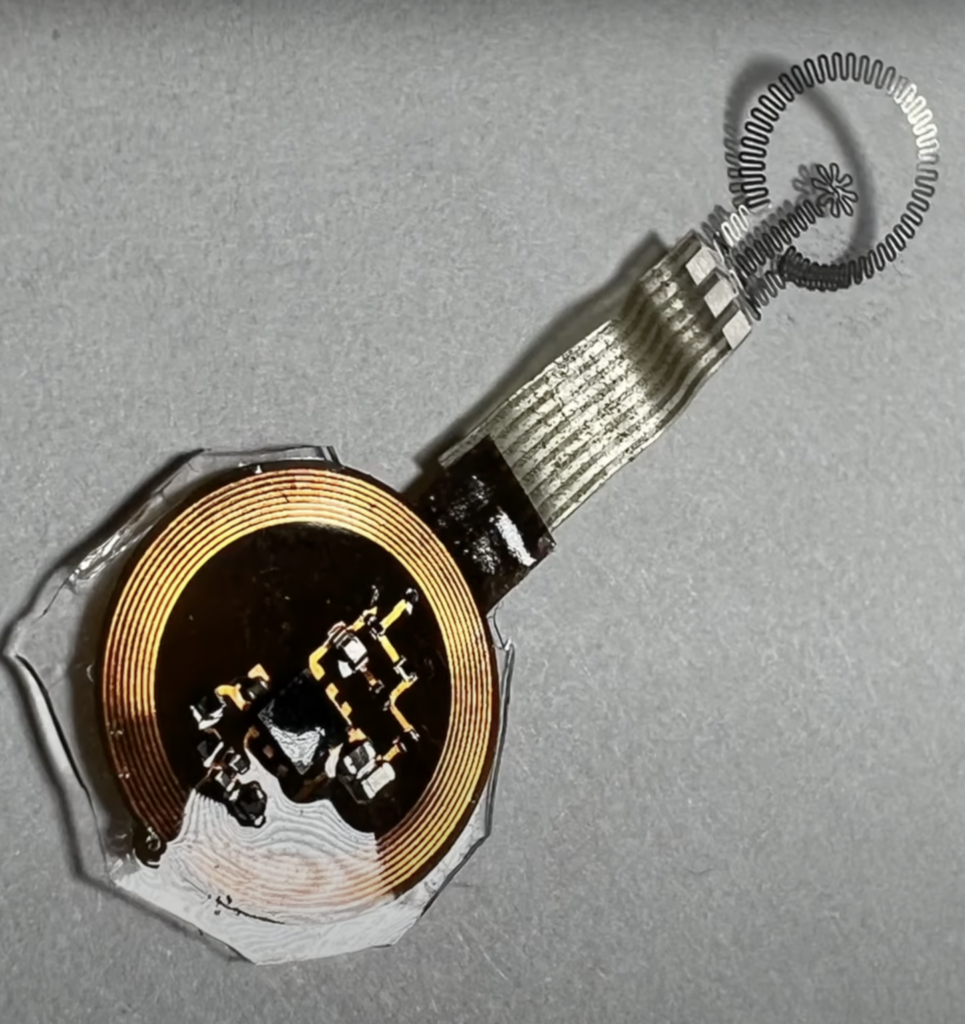
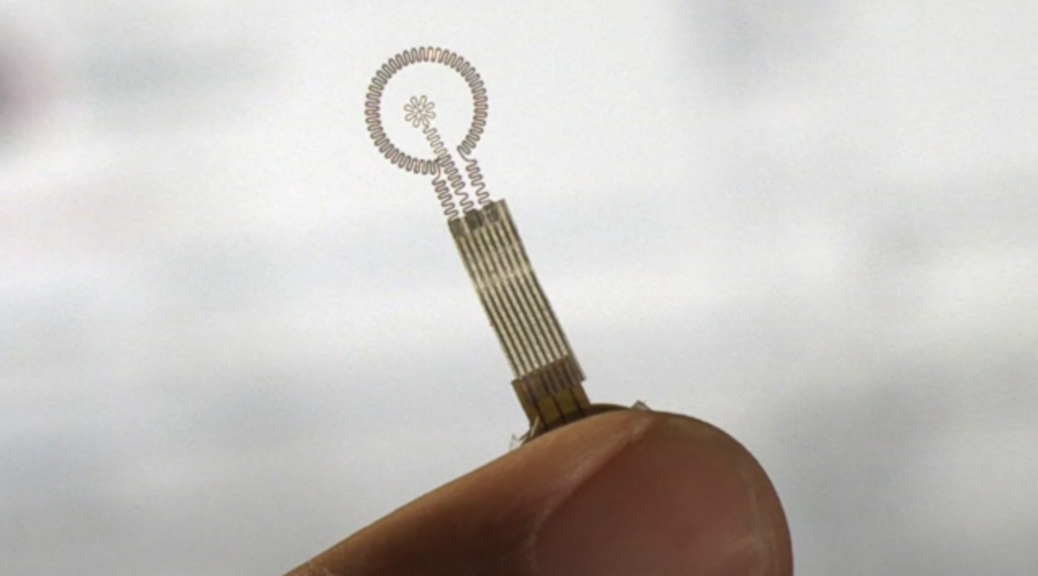
This bandage is the first of its kind. It appears small, yet is flexible and can stretch to the wound. It transfers electrodes directly to the wound.
“The electrodes are biodegradable, meaning that as the wound heals, the electrode gets embedded by your legionary tissue, and the electrodes will be gone after a year or so.”
Joseph W. Song, Northwestern University Ph.D candidate
The bioresorbable electronic method applied to the bandage allows for the electrodes to harmlessly dissolve once they are no longer needed.
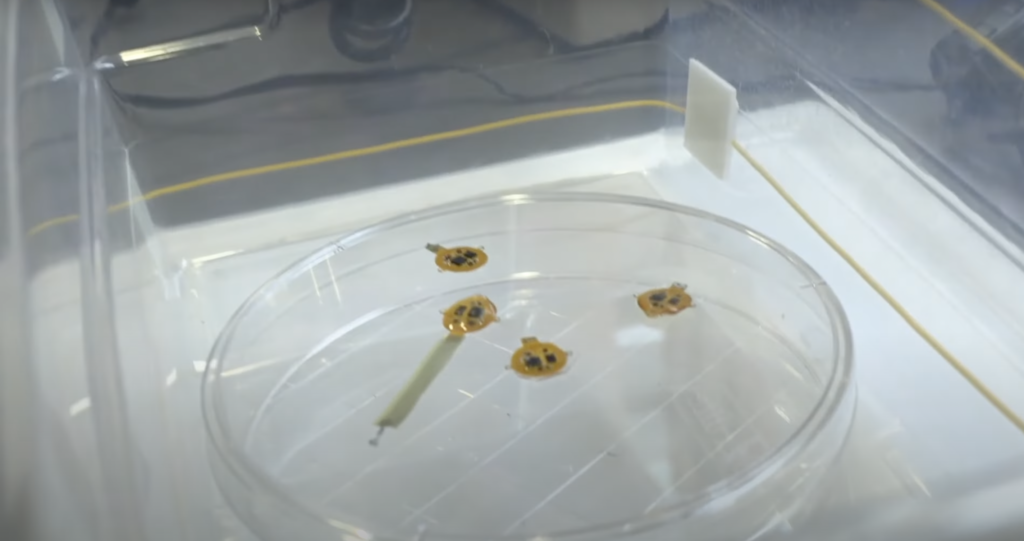
Song explained that his design and research have been in the works for around three to four years. The studies released about the bandage all come from testing on mice, in which the mice’s diabetic ulcers were healed 30% faster than normal.
The bandage works by detecting the wetness and dryness of the wound. Song explained that dryness is the key factor for the healing process, and that patients will be able to monitor the wound themselves.
“The device can be powered by a handheld power supply or you can use your cell phone to power it. So the patient can power the device whenever they want,” Song said. “They don’t have to go to the hospital or the clinic to see the doctor.”
Song revealed that they have recently moved on from testing on mice, and are now testing the device on pigs.
“After testing on pigs, maybe we can move on to human studies”
Joseph W. Song, Northwestern University Ph.D candidate
The development for the device has been quite the process. Lots of trial and error have been involved while trying to create the most efficient healing time.
“I mean, I had to, like, repeat and repeat to make sure it’s working,” Song explained. “The major challenge was to do the experiment on live, moving mice. They’re not really cooperative as you think.”
Although once the patients acquire the device they will be able to power it themselves through a cell phone, which would not require going to a hospital or clinic.
“You have to go to the clinic at first, I’m talking about the conventional electrotherapy. You apply electrical stimulation to wounds to accelerate the healing process,” Song said. “But basically, you need a large equipment to do the electrical stimulation applied to the wound area.”
The electrotherapy equipment Song refers to already exists. Although, its most common use in the medical field is in physical therapy.
Physical Therapist Assistant at Ferrell-Whited Physical Therapy Services Ann Hamilton, explained how electrotherapy is used daily in physical therapy.
“The electrodes are used mostly for pain relief, sometimes to reduce some swelling and other times to help a muscle move. Sometimes people have surgery and their muscles just don’t want to come back because they might have been injured,” Hamilton said. “So it helps get it strong enough. It’ll help the muscle to contract. So it sort of retains how it’s supposed to work.”
The machine used at Ferrell-Whited Physical Therapy Services has four electrodes that are attached to the patient’s area of pain. These electrodes are attached during the patient’s appointment, and then removed at the end of their session.
“It gets to the pain receptors in your body. And those feel-good receptors get to the brain faster than pain receptors,” Hamilton said. “So it sort of fools the brain and the body into thinking this doesn’t hurt anymore.”
While this process is the most common use of electrotherapy in pain relief, it takes a different approach than Song’s bandage. The bandage is controlled by the patient to relieve their pain, but also to heal the wound. Hamilton explains that the results of electrotherapy vary, and are usually short-term results.
“It’s usually not real long lasting. Some people say as soon as we take them off the pain is back, but others say the relief lasts all day.”
Ann Hamilton, PTA at Ferrell-Whited Physical Therapy Services
Typically physical therapy patients receiving electrotherapy treatment go in twice a week to be attached to the electrodes.
Song’s approach to electrotherapy is of a whole new realm. While the electrodes are used consistently in practices to improve pain relief, his design will also promote healing, and a constant application of electrotherapy.
Now that the mice studies are complete, Song still has big plans for the development of the device.
“I’ve redesigned the device to be applied on the pig. It’s designed for mice and mice are tiny, and we can only apply the small wounds,” Song said. “So moving onto the pig we can apply it on bigger wounds, and that’s much closer to human anatomy.”
Simone Dietz, age 83, has diabetes type two. She has had a diabetic ulcer, and explained what the healing process was like for her.
“It took a long time to heal. They did wound care on it for a little bit, and then hyper-oxygenated it,” Dietz said. “Which is when they use a hyperbaric chamber and they push more oxygen into your blood to heal the wound faster.”
Song’s electrotherapy technique for diabetic ulcers was explained to Dietz. She was shown the data, which included an increased healing time for diabetic ulcers in mice.
“I would absolutely try the electrodes if I had another ulcer. The healing process took over a month, way too long.”
Simone Dietz, diabetes type two
Overall, the device is designed to heal non-healing wounds. Song also revealed that he has further plans for the bandage that will further stop any infection.
“In the future, I also want to apply high-voltage electrodes to inhibit the growth of bacteria. So that’s also another point of view for the future studies,” Song said.